How Psychedelics Can Treat Depression
How Psychedelics Can Treat Depression
As of January 2020, more than 264 million people worldwide suffer from depression. Those numbers have skyrocketed since the pandemic. Current treatment plans usually combine medications and talk therapy, but unfortunately, the success rate for this is quite low. Studies show that antidepressants are only slightly more effective than placebos. Some studies even suggest that they are less effective over the long term. For those suffering, the thought of years of treatment before seeing tangible results can be disheartening. Fortunately, new research in psychedelic-assisted psychotherapy shows there may be a faster and more effective treatment.
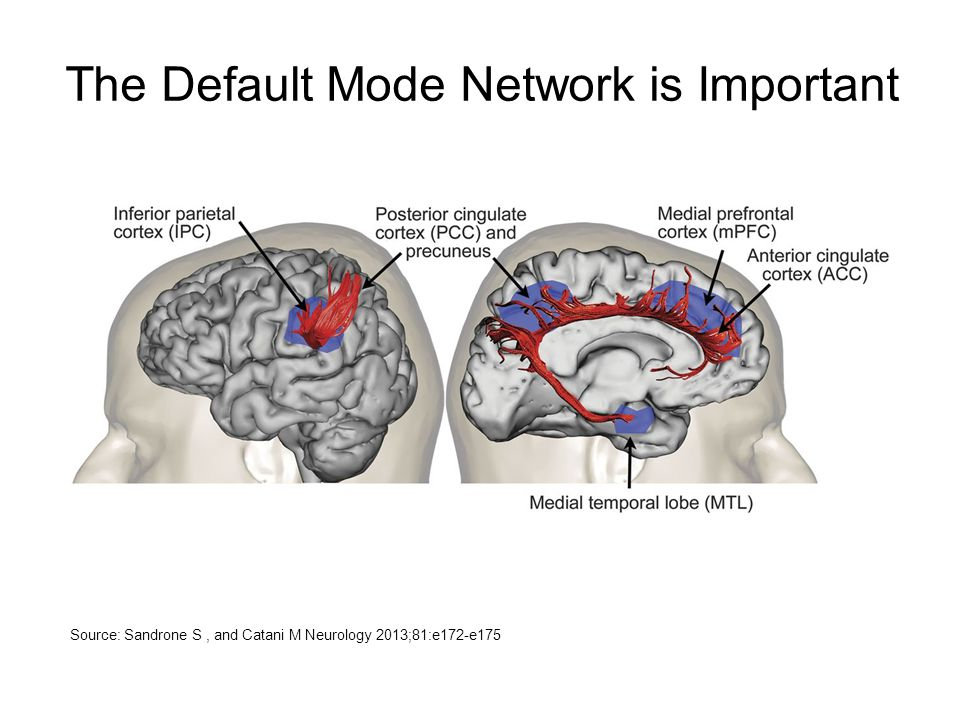
Our Default Mode
One way to think of the brain is as a predicting machine. It takes past experience and uses it as a lens through which to view the present and plan for the future. This process is important to anyone aspiring to be a functioning, effective human. Imagine if every time you encountered a
Studies show that antidepressants are only slightly more effective than placebos.
doorknob, you had to figure out from scratch how to use it. Integrating past experience into our thought process is vital. The part of our brain that does this time-saving work is made up of the medial prefrontal cortex (MPFC) and the posterior cingulate cortex (PCC). Together, they’re known as the Default Mode Network (DMN). The DMN is essentially human autopilot mode.
The Depressive Brain
A depressed brain has three main features. One is an overactive Default Mode Network (DMN). It is stuck ruminating on the past or thinking about the future. Because the DMN has evolved to help us be more efficient, an overactive DMN limits activity in other parts of the brain. The second feature is an overactive amygdala – the threat perception center, where a depressive experience is filtered through a lens of “this is harmful to you.” This reinforces narrowed brain activity, as threats need to be dealt with swiftly. The third feature is a low (depressed) activity in the emotional processing centers. These combined effects result in a brain that is literally constricted, or “narrow-minded.”
Source: Sandrone, S. and Catani, M. 2013
How Psychedelics Affect the Brain
Psychedelics, specifically psilocybin and ayahuasca, affect the brain in precisely the opposite way. Psychedelic-affected brains have decreased activity in the DMN and Amygdala and an increase in the emotional processing centers. Neuroscientists using fMRIs have shown that during these states there is an increase in connectivity between parts of the brain that do not usually communicate. Terms like “mind expansion” are now commonplace in the halls of cutting-edge laboratories.
Dr. Robin Carhart-Harris, a leading researcher in the field, offers a helpful metaphor. Imagine the mind is a ski slope, with certain paths becoming carved out as more people ski down. These paths are akin to thought and behavior patterns, which become more and more entrenched as people age. The more entrenched the pattern, the harder it is to change or to even see the possibility of change. Taking a
Taking a psychedelic, he explains, is like shaking the snow globe.
psychedelic, he explains, is like shaking the snow globe. For the duration of the psychedelic experience, the snow becomes level again, and all paths are available. With the help of a trained psychotherapist, this is an opportunity to begin new thought patterns and erase old ones. Eventually, the snow settles again, hopefully with healthier patterns in place.
Psilocybin-Assisted Psychotherapy for Depression
Psilocybin is the compound found in what is commonly referred to as “magic mushrooms.” Psilocybin–assisted psychotherapy generally involves preparatory sessions, two or three psilocybin sessions one week apart, and integration sessions. One study tested the effects on patients with treatment-resistant depression. The results were extremely promising. All participants showed some level of immediate and enduring alleviation of depression symptoms as measured by standard clinical assessments. After one week, 67% had a complete remission of depression symptoms. And three months later, 40% were still in remission.
Those who suffer from depression describe it as a constant loop of negative thoughts, an oppressiveness, and a heaviness in the brain. One patient described their experience of psilocybin-assisted psychotherapy: “Your mind is always chattering and observing things, and that was all shut down. For me, there was a feeling of new space…I got a new positivity that I didn’t have for some time.”
The effectiveness of psilocybin-assisted psychotherapy is unprecedented in the treatment of depression. Other major positives are a virtual lack of any side effects and the relatively minimal number of required sessions. This is especially promising when compared to the efficacy of conventional treatment plans. Patients only respond to antidepressant medications after two months on average. The majority stop after one month due to ineffectiveness plus the myriad side effects, including nausea, weight gain, decreased libido, fatigue, fogged thinking, and many others. In contrast, psilocybin-assisted psychotherapy works immediately and with lasting results.
Victor de Schwanberg/Science Photo Library/Newscom
Ayahuasca-Assisted Psychotherapy for Depression
Another psychedelic that’s shown promising results in treating depression is ayahuasca. This compound is made by combining different organic materials native to the Amazon Basin. Ayahuasca has a long history of use in shamanistic rituals by indigenous peoples, practiced there for hundreds or even thousands of years. Only recently, however, did it become known in the West. So Ayahuasca’s legality is tricky in the United States and Canada, which is why there are many ayahuasca retreats around the world.
The ayahuasca group had significantly lower depression symptoms immediately after the experience.
One study led by Brazilian researchers investigated the effects of ayahuasca on treatment-resistant depression patients. The patients took a single dose of ayahuasca, with the experience lasting about eight hours. When compared with a control group, both groups had reduced depression symptoms following the session. However, the ayahuasca group had significantly lower depression symptoms immediately after the experience. In addition, the ayahuasca group had a significantly more enduring response rate. This response rate (64%) is nearly double the average response rate of ketamine (7-35%), another psychoactive compound often used in treating depression.
Brian Lissak is the Director of Ketamine-Assisted Psychotherapy at Behavioral Associates, a private practice mental health office in Manhattan.
Gallery
Recent Articles
Drug Addiction Treatment
•
July 14, 2025
Loading...
Bebaloncar Charts New Terrain with “Words,” the Hypnotic First Single from Love to Death
- Georgia P. Taylor
Vinyl Relics: Before The Dream Faded by The Misunderstood
- Farmer John